A) AGING
The natural aging process affects all tissues in a progressive manner. The nervous system is no exception. Older people lose their sight, hearing, smell and even taste. But they also find their sense-performance decreasing on the whole. Fine touch, temperature and pain are senses that undergo changes with aging. In many cases a usually innocuous stimulus becomes a painful and uncomfortable sensation, which we call allodynia. The common view is that as we age, we lose a considerable amount of sensory receptors and that this is the cause for sensory dysfunction. Some pathologies such as diabetes can accelerate the degeneration of nerves and aggravate the process, indeed even causing chronic and painful ulcers on the skin.
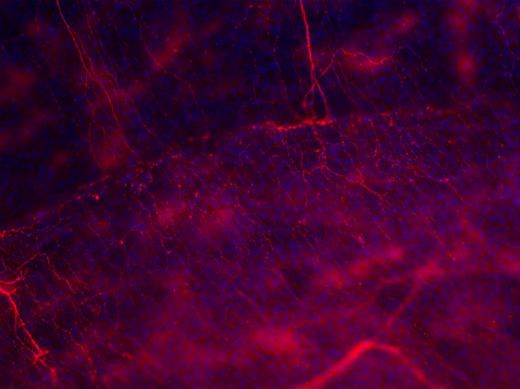
However, not all structures appear to be equally vulnerable to aging. In our laboratory we have studied sensorial innervation of the ocular surface in aging mice and have focused on the analysis of cold-sensitive receptors, due to their special importance in the regulation of tear-secretion. We have identified and characterised both functionally and molecularly, cold-receptor neuron populations that feature the TRPM8 ionic canal in the cornea. Furthermore, these two sorts of neurons have different functions. The first type plays a regulatory role in the production of tear secretions and we believe that it contributes to the blocking of pain by inhibiting other poly-modal neurons. The second kind displays typical characteristics of a classical nociceptor. With focus being solely on these two nerve-fibre types of the cornea, we observed that aging affects each of them in a different manner, with interesting singular degenerative processes in the cornealafferents: degeneration linked to aging in the cold fibres takes place almost exclusively in the first of the two fibre types, while the other type is not significantly affected. The selective disappearance of the “regulator” kind of TRPM8 fibres, is linked to dysfunction of the tear-duct. The “nociceptor” type of the TRPM8 fibres remains present in older animals display pain and inflammation markers. In accordance with our hypothesis, the latter would be responsible for the appearance of bothersome and painful sensations that go in hand with tear-duct dysfunction, in patients of advanced age. Similarly, in aging animals we find an electrical activity in a population of cold-terminal population that appears similar to that of the regulator fibres (which in normal conditions has a constant basal activity level) but with a response activity that is higher and more prolonged, similar to that of poly-modal fibres.
In this way, we have been able to directly link selective loss of nerve fibres in the cornea to tear-duct dysfunction associated with aging, in a model that accurately reflects the pathological signs of the dry eye: tear-duct dysfunction, inflammation and pain.
The dual activity of the TRPM8 canal defines it as a therapeutic target for solving neuropathic and inflammation-related pain.
On the other hand, understanding the reason for which a type of neuron so restricted displays greater vulnerability to degeneration, opens avenues for the design of neuro-protective treatments.